Submitting a Claim to Green Shield when Three or More Intervention Codes are Needed
When co-ordinating a claim with the provincial plan and Green Shield, three or more intervention codes may be required to submit the claim to Green Shield. This can occur when the patient's funding request is pending approval or has been rejected by the provincial plan.
As CPHA claim standard does not permit more than two intervention codes to be entered for a claim, one of the following intervention codes can be entered for Green Shield along with the DA intervention code to bypass the other required codes:
-
SX - Pending provincial plan, bypass other programs
-
SW - Rejected by provincial plan, bypass other programs
For more information on Green Shield response and intervention codes, click here.
Example 1 - Provincial Funding is Pending
A claim for a high cost (over $1000) EAP drug needs to be submitted to Ontario Drug Benefit and Green Shield. A request has been submitted for funding under EAP and it is pending approval. In this scenario, the DA, MP, and DX codes are required to submit the claim to Green Shield. To adjudicate the claim to Green Shield:
-
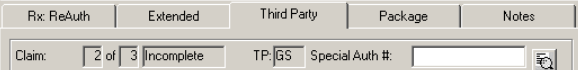
In Rx Detail, select the Third Party tab.
-
Navigate to GS third party.
-
Select Add.
-
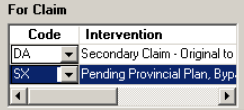
Select SX - Pending provincial plan, bypass other programs. Confirm the DA intervention code is entered.
-
Select Fill.
Example 2 - Provincial Funding Request has been Rejected
A vacation supply for a high cost (over $1000) EAP drug needs to be submitted to Ontario Drug Benefit and Green Shield. A request has been submitted for funding under EAP and it has been rejected. In this scenario, the DA, MP, MV, and DW codes are required to submit the claim to Green Shield.
To adjudicate the claim to Green Shield:
-
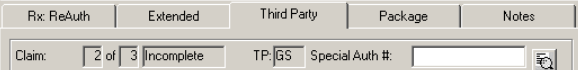
In Rx Detail, select the Third Party tab.
-
Navigate to GS third party.
-
Select Add.
-
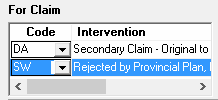
Select SW - Rejected by provincial plan, bypass other programs. Confirm the DA intervention code is entered.
-
Select Fill.